As an innovator in the oncology field, Green Bay Oncology
has created a solid financial counseling program to ensure that no patients have to carry the financial burden that may accompany a cancer diagnosis by themselves. By sharing our story, the financial counseling team hopes other cancer programs can benefit from our experiences to either develop their own financial counseling services or to enhance existing services.
Our Story
The financial counseling position at Green Bay Oncology began as a 1 person team 10 years ago when our group consisted of 7 physicians and 6 clinic locations. At a time when prior authorizations for IV chemotherapy were still unheard of, the financial counselor’s basic responsibilities consisted of meeting with uninsured patients who needed to start treatment and working with the pharmaceutical companies to get free drug, if available. Over the next few years, however, the financial counselor position continued to grow along with patient demand and began to include assistance for oral anti-cancer agents as well.
Given the growing complexity of cancer care, along with the increase in the number and cost of oral anticancer therapies, it is no surprise that the financial counselor program quickly became an important part of Green Bay Oncology. In 2015, Green Bay Oncology aligned with Hospital Sisters Health System St. Vincent Hospital, becoming part of the regional cancer center and making us the largest oncology group in northeast Wisconsin.
Today, we have a team of 6 counselors assisting 9 medical oncologists, 3 pediatric oncologists, 3 radiation oncologists, 1 gynecology oncologist, 8 nurse practitioners, and 3 physician assistants across 6 cancer center locations in northeast Wisconsin and the Upper Peninsula of Michigan.
In our comprehensive cancer program, financial counselors follow patients from the start to the completion of their treatment journey and are an integral part of the patient’s experience. We act as a liaison between the patient, the provider, and other clinic departments, as well as the patient’s insurance carrier. Efficient communication between all of these individuals and departments is the core of our program’s success.  We are also fortunate to have providers who understand the key message concerning financial toxicity and its potential to impact patient outcomes.
We are also fortunate to have providers who understand the key message concerning financial toxicity and its potential to impact patient outcomes.
“Medicine in general, and oncology in particular, used to believe that money shouldn’t be a consideration in treatment,” said Green Bay Oncology provider Mitch Winkler, MD. “This led us to act as if ‘money was no object’ where cancer treatment was concerned. We feared that considering financial factors would harm our patients or impede their care. But by neglecting financial factors in cancer treatment, we’ve exposed our patients to terrible harm.”
Our Process
The financial counselor’s job begins before the patient steps foot in our clinic. Acting as an advocate for patients, our benefits specialist will first verify their insurance benefits to ensure patients are in-network with our physicians.
Once treatment is prescribed, whether IV, oral, or radiation therapy, the financial counselor will immediately verify that the treatment is indicated for the patient’s diagnosis, checking the National Comprehensive Cancer Network (NCCN) Compendium and/or the Medicare Compendium.
Next, we verify whether the patient’s insurance requires prior authorization. If so, we initiate the authorization process immediately to ensure that treatment can start within three to five days.
Once we’ve obtained the authorization approval, we continue to follow the patient to ensure that if treatment continues longer than anticipated, the approval does not lapse. We are able to generate a notification in our electronic health record (EHR) that will alert us of an expiring authorization two weeks before the expiration date. We can then go into the patient’s chart and determine if re-authorization is needed.
For patients treated with oral therapies, our financial counselors initiate the first prescription fill with specialty pharmacy to verify insurance approval and make sure the medication is affordable for the patient. The financial counselors first meet with patients while they are in the clinic, explain how specialty/mail-order pharmacies operate and—depending on their insurance—discuss co-pay assistance.
After meeting with the patient, we fax the prescription along with the patient’s demographics, current medication list, and copies of insurance cards to our single point of contact at the specialty pharmacy. Because we have a pre-existing relationship with this point of contact, communication is often quick and easy, helping to ensure that the medication gets to the patient in a timely manner.
Our pharmacy contact will notify us if an authorization is required. Once we receive that notification we then submit to the insurance company for the approval. When approval has been obtained, we notify the pharmacy and the financial counselor is then given a date when the patient is scheduled to receive his or her medication. We then verify that the patient has an appointment scheduled for a toxicity evaluation within 10 days from the date the medication is received.
Financial Assistance for IV & Oral Therapy
If the physician is ordering a treatment that is not yet FDA approved for the patient’s diagnosis, or not indicated (i.e., off-label), we will always try to get approval through the insurance company first. If we receive a denial from the insurance company, we then go straight to the pharmaceutical company and apply to the patient assistance program in hopes to receive free drug assistance for our patients. We do not ask patients to fill out any patient assistance forms; all forms are completed and sent in by the financial counselor. All that is needed from patients is their signature and, if required, income documentation to ensure eligibility.
When patients are first diagnosed and prescribed treatment, one of their first concerns is usually “How am I going to afford this?” Most will have insurance to assist them with their treatments and appointments but, as we all know, the out-of-pocket maximums on insurance plans just keep getting larger. It is important to meet with patients before they start treatment and discuss cost and options to help alleviate any financial burdens of cancer treatment.
Depending on the type of treatment, we will go over options, such as foundation assistance on the national level (Patient Advocate Foundation, Patient Access Network Foundation, CancerCare, etc.) or on the local level. For example, in northeast Wisconsin we have some great local foundations, such as Ribbon of Hope and the Ovarian Cancer Community Outreach (OCCO), to help reduce not only treatment costs, but everyday living costs as well.
Once approved, we will add these foundations to the patient’s EHR and take care of all submissions for payment. Claims are sent to the foundation before patients receive a bill. This process is in place to alleviate as much of the financial burden as we can from patients in hopes of reducing any anxiety caused by additional bills and/or collection phone calls.
For commercially-insured patients who do not qualify for foundation assistance and/or for whom there are no funds available for their diagnosis, we will turn to pharmaceutical company co-pay cards. These drug-specific cards can be a great option for reducing out-of-pocket costs. There is no income limitation for these cards so long as patients give us their consent to enroll them; financial counselors can take care of everything, including submitting charges on their behalf.
In 2015 alone, we saved our patients $573,328.50 on their oral chemotherapy co-pays. This amount is only from three of the main specialty pharmacies we use: Accredo, Diplomat, and Community Pharmacies. Recently, in 2016, the financial counseling team worked closely with the hospital’s charity foundation and reached out to donors to create a specific fund for our patients on oral therapy that could be used when all other foundation funds were exhausted.
With the constant increase of insurance plans’ yearly out-of-pocket maximums, the amount of money our program saves our patients each year continues to grow. Figure 1, page 7, illustrates exactly what was paid to our clinic from foundations and pharmaceutical co-pay cards. This does not reflect the full grant amount that was issued to patients. In 2015, between IV and oral chemotherapy assistance, the financial counselors at Green Bay Oncology saved patients more than 1 million dollars!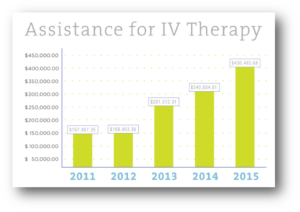
Financial Assistance for Radiation Oncology
Unfortunately the radiation oncology world is a little bit different in terms of financial assistance. There is very limited access to patient assistance for radiation oncology patients when it comes to treatment; for that reason we like to meet with these patients before they start radiation therapy.
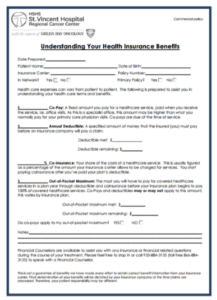 Our financial counselors provide patients with an overview of their insurance coverage, including their out-of-pocket responsibility, what they’ve met, and how much they have remaining. Also, specific forms (see page 5) are given to each patient, depending on their type of coverage, i.e., commercial, Medicare Advantage, or Medicare and a supplement. This information helps give patients an idea of how much they may be responsible for.
Our financial counselors provide patients with an overview of their insurance coverage, including their out-of-pocket responsibility, what they’ve met, and how much they have remaining. Also, specific forms (see page 5) are given to each patient, depending on their type of coverage, i.e., commercial, Medicare Advantage, or Medicare and a supplement. This information helps give patients an idea of how much they may be responsible for.
We also talk to these patients upfront regarding payment plans, as well as Community Care/Charity Care if they feel this is something they would be eligible for. Patients are also made aware that a financial counselor will be given their treatment plan in order to verify that everything is indicated and authorized prior to their beginning therapy.
Due to the success of these forms in our radiation oncology department, our goal is to meet with and provide these same benefits to all patients in the medical oncology clinic by 2017.
At Green Bay Oncology, our financial counselors do not just handle the above-mentioned duties. Financial counselors are constantly involved in projects, creating new processes and building teams within other departments to continue driving our cancer program forward.
Financial counselors work closely with social workers and nurse navigators to make sure patients are taken care of both inside and outside of the clinic, including ensuring patients have all the necessary appointments scheduled, transportation to and from the clinic, or assistance to help with everyday bills that seem to take a backseat when medical bills start accumulating.
Our team also works with outside resources to enroll eligible patients in Medicaid. Financial counselors can also refer underinsured patients to the proper resources to gain the additional coverage they need going forward, such as Medicare supplemental plans and/or prescription coverage (Medicare Part D). The open communication between departments is a prime example of how our cancer program strives to always put patients first. Financial counselors work closely with physicians to develop and continually update clinical pathways. These disease-specific pathways help standardize our approach to how we treat our patients while showing payers that we are consistent in our treatment plans. Counselors verify that all treatments are listed in the NCCN Compendium while taking into consideration the cost of the therapy—not only for the patient, but also for the clinic.
The financial counselors are the patient’s direct point of contact for any and all billing concerns. Patients are instructed to call their financial counselor with any questions or concerns they may have once they start receiving bills. We work with patients to set up payment plans tailored to their comfort level.
Community Care applications are also given to patients once all other assistance options have been exhausted. Some factors taken into consideration while processing Community Care applications include annual household income, household size, assets and debt information, and the past three months of bank statements. Once the signed application and all required financial documentation are returned, financial counselors process these and inform patients of the amount of assistance for which they have been approved.
On top of all medication authorizations, including chemotherapy and retail prescriptions, our team also authorizes any radiology imaging that is ordered by providers, as well as molecular lab testing such as chromosome analysis, BCR/ABL, and JAK2 orders. It’s very important to verify coverage for any testing ordered by physicians to prevent that financial burden from falling into our patients’ laps.
When our clinic does receive a denial from a payer on any physician-ordered treatment, it is our financial counseling team’s responsibility to appeal. We will draft a letter to send to the payer along with all supporting documentation, such as compendium listings, FDA indications, insurance policies, etc. Our team is proud to say it’s not very often that the denials are upheld once our appeals are submitted.
Working for a hospital system that understands the need for financial counselors is imperative. We hear far too often while attending conferences around the region that cancer programs are trying to “prove” to their leadership that a financial counselor position is feasible. We think to ourselves, “What? You have to prove it?” Don’t the numbers speak for themselves? Institutions that do not think they need financial counselors should answer these questions:
• What does your Patient A/R (Accounts Receivable) stand at?
• How are your patients affording their treatments?
• How much are you writing off as charity?
• How many patients are you sending to collections?
Financial counseling is not only a service to assist the patients; it also guarantees the clinic is going to get paid. It’s 2017 and the cost of care is going to continue to climb. Committing as a practice or program to be financially responsible to patients has to be at the forefront.
By attending multiple ACCC meetings (the Financial Advocacy Network [FAN] Meetings, Oncology Reimbursement Meetings [ORMs], and the National Oncology Conference) our financial counselors have experienced ample opportunity for networking with other clinics across the country who have continually expressed their desire to learn more about our comprehensive financial counseling program. We have provided consulting services to several other cancer programs in Wisconsin and Michigan, helping them replicate our financial counselor position within their own program. ACCC meetings have opened our eyes to the fact that there are far too many cancer programs that are unaware of how they can help mitigate financial toxicity for their patients. It is vital for us to educate the cancer community on the importance of financial toxicity prevention. Won’t you join us?
Gretchen Van Dyck is a financial counselor, Green Bay Oncology at HSHS St. Vincent Hospital Regional Cancer Center in Green Bay, Wisconsin
To view the complete ACCC Patient Assistance & Reimbursement Guide 2017: click here